If you have visitied a doctor frequently, chances are that they viewed or input data about your health on a computer screen. That’s because they were likely reading and updating your information on your electronic health record (EHR). In this article, we’ll explain exactly what an EHR is, the benefits of using them in healthcare settings and how to implement an EHR system.
What is an EHR system?

An electronic health record (EHR) is a digital version of a patient’s paper chart. EHRs are real-time, patient-centered records that make information available instantly and securely to authorized users. While an EHR does contain the medical and treatment histories of patients, an EHR system is built to go beyond standard clinical data collected in a provider’s office and can be inclusive of a broader view of a patient’s care. EHRs are a vital part of health IT and can:
- Contain a patient’s medical history, diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory and test results
- Allow access to evidence-based tools that providers can use to make decisions about a patient’s care
- Automate and streamline provider workflow
One of the key features of an EHR is that health information can be created and managed by authorized providers in a digital format capable of being shared with other providers across more than one health care organization. EHRs are built to share information with other health care providers and organizations – such as laboratories, specialists, medical imaging facilities, pharmacies, emergency facilities, and school and workplace clinics – so they contain information from all clinicians involved in a patient’s care.
Benefits of Electronic Health Records
 EHRs are real-time, patient-centered records that make information available instantly and securely to authorized users. While an EHR does contain the medical and treatment histories of patients, an EHR system is built to go beyond standard clinical data collected in a provider’s office and can be inclusive of a broader view of a patient’s care. EHRs can:
EHRs are real-time, patient-centered records that make information available instantly and securely to authorized users. While an EHR does contain the medical and treatment histories of patients, an EHR system is built to go beyond standard clinical data collected in a provider’s office and can be inclusive of a broader view of a patient’s care. EHRs can:
- Contain a patient’s medical history, diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory and test results
- Allow access to evidence-based tools that providers can use to make decisions about a patient’s care
- Automate and streamline provider workflow
Types of EHR Implementation
When implementing an Electronic Health Record (EHR) system, healthcare organizations have two primary options: local/in-house deployment or cloud-based solutions. Each approach has its own characteristics and considerations.
1. Local/In-house Implementation:
- In the local/in-house model, the EHR application is deployed on local servers within the healthcare organization’s premises. Here are some key features:
- Data is stored and managed within the organization, providing direct control over security and privacy.
- The system can function even without an internet connection, ensuring uninterrupted access to patient records.
- On-premises IT support is required to maintain and manage the infrastructure, including software updates, license fees, and maintenance.
- Backup and disaster recovery processes may be less robust compared to cloud-based solutions.
2. Cloud-based Implementation:
Cloud-based EHR systems rely on third-party vendors or Managed Service Providers (MSPs) that host and manage the EHR application. Here are some key features:
- Accessible from multiple devices and locations, allowing healthcare providers to securely access patient data from anywhere with an internet connection.
- Cost-effective, as it eliminates the need for significant upfront investments in hardware and infrastructure. Instead, healthcare organizations typically pay a subscription fee for the cloud service.
- Data is stored in external cloud servers, providing built-in backup and disaster recovery capabilities.
- The reliance on a third-party vendor for support and maintenance requires trust and a robust service level agreement (SLA) to ensure data security and system availability.
Both local/in-house and cloud-based EHR implementations have their pros and cons. Healthcare organizations should carefully consider their specific needs, resources, security requirements, and long-term scalability when choosing the most suitable implementation approach for their EHR system.
Threats to EHR Systems
Phishing Attacks
Attacker will exploit email, attempting to trick the user into reveling login credentials or installing malicious software onto the EHR system/network.
Malware and Ransomware
Deployed onto a user system in a number ways (phishing, exploits, etc.), malware can impact EHR data; stealing, destroying or holding the data for ransom.
Cloud threats
Cloud services represent a new factor in supply chain/third party exploitation, giving hackers a larger attack surface in which to compromise an EHR system.
Insufficient Encryption
Many devices on the EHR network use little or no encryption, which makes data in transit vulnerable to exploitative attacks, such as Man-in-the-Middle and other exfiltration methods.
Employees/Insider Threats
Personnel within the organization, whether through unwitting negligence or malicious intent, can cause significant damage, using held credentials to gain access to EHR data system.
EHR Cloud
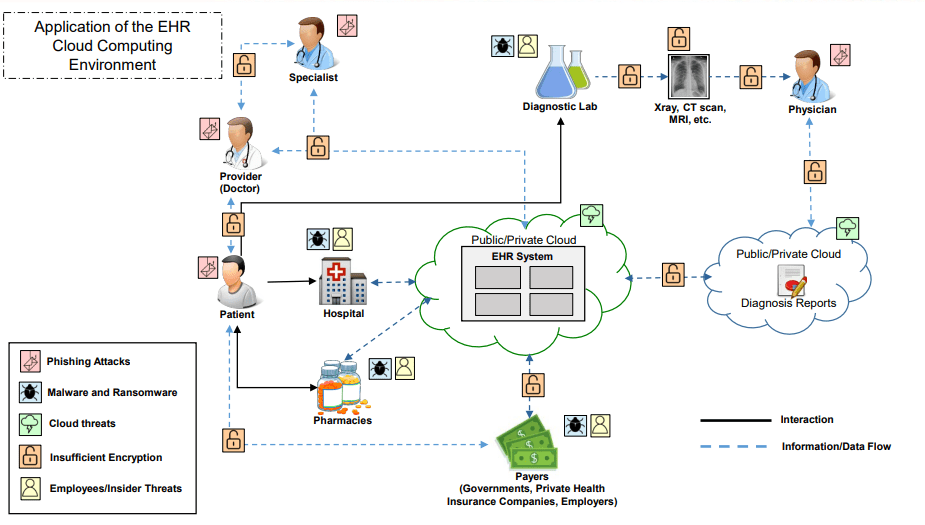
Source: Aircse
Figure 1: Application of cloud computing environment
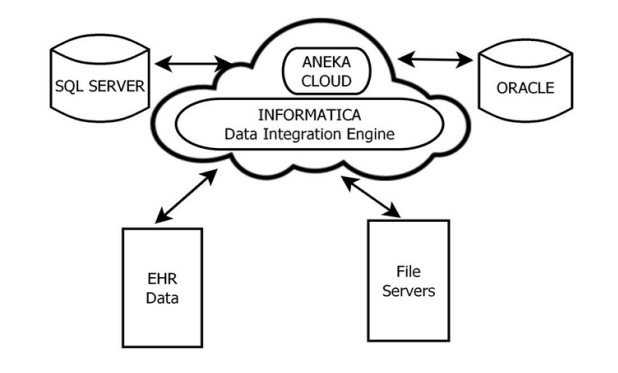
Figure 2: Data intergration approach
With the current increase of clinical data the problems of how to collect data from scattered and different systems and how to analyze the big scale clinical data become cavilling. Data integration approaches for collecting clinical data from scattered and different health IT systems will lead to more effective healthcare applications. Approaches for large scale clinical data analytics will lead in development of more effectual healthcare applications, improve the quality of predictions and in timely decision making. The proposed Information Integration and Informatics framework allows healthcare data accumulation and organization from different stakeholders(doctors, patients, payers, specialists, physicians etc) as in Fig.1 and disparate data sources( databases, unstructured and structured formats, etc)as in Fig.2. With Information Integration and Informatics framework healthcare data can be safely exchanged between different stakeholders to assist more accurate and timely healthcare delivery.
How To Implement an EHR system
If your healthcare practice is considering getting an EHR system, it’s best to follow these steps to ensure the right decisions are made.
1. Assess your organizational readiness: The first EHR implementation step is to assess your current organization – its goals, needs, and financial and technical readiness. With an accurate view of your preparedness, your organization can design an EHR implementation plan that meets the specific needs of your organization.
2. Plan Your Approach: In the planning phase, draw on the information you gathered during the assessment phase to outline your organization’s EHR implementation plan. Remember to look at all aspects of your organization from an electronic point-of-view.
3. Select or Upgrade to a Certified EHR: Next you should select or upgrade to a certified EHR. Your EHR implementation team should use the information gathered in the assessment and planning phases to choose the right EHR for your organization.
4. Conduct Training & Implement an EHR System: During this phase of EHR implementation, your organization should install the EHR system. You’ll also need to make sure you prepare for EHR implementation go-live, so include training, pre-go-live dress rehearsals, and pilot testing in this step.
5. Plan Your Go-live Lead-up: Going live with a new system is a big deal, so it’s important to have plans and protections in place leading up to it. For example, you should:
- Determine system testing needs before and immediately after you go live
- Figure out how much downtime there will be if any during the transition between systems
- Make a plan for communicating your change in systems to current patients
- Backup your data as a fail-safe
6. Continue Quality Improvement: Once you’ve implemented an EHR and achieved meaningful use, you should continuously evaluate and improve. Revisit your organization’s goals and needs to continue refining workflows and improving patient outcomes.
Conclusion
Electronic Health Records (EHRs) have revolutionized the accessibility of medical records, providing healthcare providers with instant access to crucial patient information and enabling them to deliver better and more efficient care. With EHRs, providers can gain valuable insights into a patient’s treatment history, diagnoses, medications, and other critical data, allowing for more informed decision-making and personalized care plans. The seamless access to EHRs has improved care coordination, reduced medical errors, and enhanced patient outcomes. EHRs have truly transformed the healthcare landscape, empowering providers to deliver timely, accurate, and patient-centered care.





